From the article you will learn the features of varicose veins of the small pelvis in women - this is a deformation of the veins of the pelvic region with impaired blood flow in the internal and external genital organs.
General Information
In the literature, varicose veins of the small pelvis are also referred to as "pelvic congestion syndrome", "varicocele in women", "chronic pelvic pain syndrome". The prevalence of varicose veins in the small pelvis increases in proportion to age: from 19. 4% in girls under 17 to 80% in perimenopausal women. Most often, the pathology of the pelvic veins is diagnosed in the reproductive period in patients in the age group of 25-45 years.
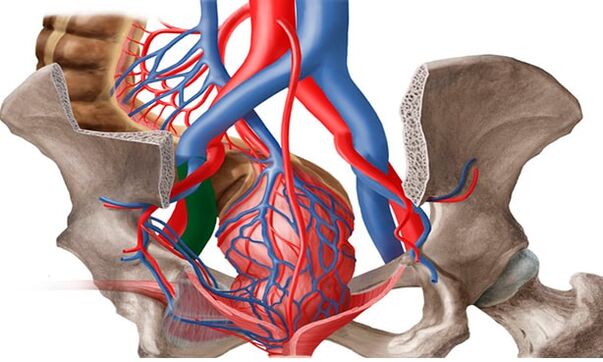
In the vast majority of cases (80%), varicose transformation affects the ovarian veins and is extremely rare (1%) observed in the veins of the broad ligament of the uterus. According to modern medical approaches, the treatment of VVMT should be carried out not so much from the point of view of gynecology, but, first of all, from the point of view of phlebology.
Pathology triggers
Under the varicose veins of the pelvic organs in women, doctors understand a change in the structure of the vascular walls characteristic of other types of the disease - weakening followed by stretching and the formation of "pockets" within which blood stagnates. Cases in which only the vessels of the pelvic organs are affected are extremely rare. In about 80% of patients, along with this form, there are signs of varicose veins of the inguinal veins, vessels of the lower extremities.
The incidence of varicose veins of the small pelvis is more pronounced in women. This is due to anatomical and physiological features, which suggest a tendency to weaken the venous walls:
- hormonal fluctuations, including those associated with the menstrual cycle and pregnancy;
- increased pressure in the small pelvis, typical of pregnancy;
- periods of more active filling of the veins with blood, including cyclical menstrual periods, during pregnancy and during sex.
All these phenomena belong to the category of factors that provoke varicose veins. And they are found exclusively in women. The greatest number of patients are faced with varicose veins of the small pelvis during pregnancy, as there is a simultaneous stratification of provoking factors. According to statistics, among men, varicose veins of the small pelvis are 7 times less common than in the fair sex. They have a more diverse set of provoking factors:
- hypodynamia - long-term preservation of low physical activity;
- increased physical activity, especially dragging weights;
- obesity;
- lack of sufficient fiber in the diet;
- inflammatory processes in the organs of the genitourinary system;
- sexual dysfunction or a lucid refusal to have sex.
A genetic predisposition can also lead to the pathology of the plexuses located inside the small pelvis. According to statistics, varicose veins of the perineum and pelvic organs are most often diagnosed in women whose relatives have suffered from this ailment. The first changes in them can be observed in adolescence during puberty.
The greatest risk of developing inguinal varicose veins in women with involvement of the pelvic vessels is observed in patients with venous pathology elsewhere in the body. In this case, we are talking about congenital weakness of the veins.
Aetiopathogenesis
Proctologists believe that the following main reasons always contribute to the occurrence of VVP: valvular insufficiency, venous obstruction, and hormonal changes.
Pelvic venous congestion syndrome can develop due to the congenital absence or insufficiency of the venous valves, which was revealed by anatomical studies in the last century, and modern data confirm this.
It was also found that in 50% of patients, varicose veins are genetic in nature. FOXC2 was one of the first genes identified that play a key role in the development of VVP. Currently, the relationship between disease development and genetic mutations (TIE2, NOTCH3), thrombomodulin level and transforming growth factor type 2 has been determined. These factors contribute to a change in the structure of the valve itself or the venous wall - all this leads to the failure of the valve structure; widening of the vein, which causes a change in the function of the valve; to progressive reflux and finally to varicose veins.
An important role in the development of the disease can be played by connective tissue dysplasia, the morphological basis of which is a decrease in the content of various types of collagen or a violation of the relationship between them, which leads to a decrease in venous strength.
The incidence of VVP is directly proportional to the amount of hormonal changes, which are especially pronounced during pregnancy. In pregnant women, the capacity of the pelvic veins increases by 60% due to the mechanical compression of the pelvic vessels by the pregnant uterus and the vasodilating effect of progesterone. This venous dilation persists for one month after delivery and can cause venous valve failure. Also, during pregnancy, the mass of the uterus increases, its position changes occur, which provoke stretching of the ovarian veins, followed by venous congestion.
Risk factors also include endometriosis and other inflammatory diseases of the female reproductive system, estrogen therapy, adverse working conditions for pregnant women, which include hard physical work and prolonged forced position (sitting or standing ) during the working day.
The formation of varicose veins in the small pelvis is also facilitated by the anatomical features of the outflow from the veins of the small pelvis. The diameter of the ovarian veins is usually 3-4 mm. The long, thin ovarian vein on the left flows into the left renal vein and on the right into the inferior vena cava. Normally, the left renal vein is located in front of the aorta and behind the superior mesenteric artery. The physiological angle between the aorta and the superior mesenteric artery is approximately 90 °.
This normal anatomical position prevents compression of the left renal vein. On average, the angle between the aorta and the superior mesenteric artery in adults is 51 ± 25 °, in children - 45. 8 ± 18. 2 ° in boys and 45. 3 ± 21. 6 ° in girls. In the case of a decrease in the angle from 39. 3 ± 4. 3 ° to 14. 5 °, aorto-mesenteric compression or nutcracker syndrome occurs. This is the so-called anterior, or true, nutcracker syndrome, which has the greatest clinical significance. Posterior nutcracker syndrome occurs on rare occasions in patients with a retroaortic or annular arrangement of the distal left renal vein. Obstruction of the proximal venous bed causes an increase in pressure in the renal vein, which leads to the formation of renoovarian reflux in the left ovarian vein with the development of chronic pelvic venous insufficiency.
May-Turner syndrome - compression of the left common iliac vein by the right common iliac artery - also serves as one of the etiological factors of varicose veins in the pelvis. It occurs in no more than 3% of cases, is most often found in women. Currently, due to the introduction into practice of radiation and endovascular imaging methods, this pathology is detected more and more often.
Classification
Varicose veins are divided into the following forms:
- The main type of varicose veins - an increase in the blood vessels of the pelvis. The reason is valvular insufficiency of 2 types: acquired or congenital.
- The secondary form of thickening of the pelvic veins is diagnosed only in the presence of gynecological pathologies (endometriosis, neoplasms, polycystic).
Varicose veins in the pelvis develop gradually. In medical practice, there are several main stages in the development of the disease. They will differ depending on the presence of complications and the spread of the disease:
- First degree. Changes in the structure of the valves of the ovarian veins can occur for hereditary reasons or be acquired. The disease is characterized by an increase in the diameter of the veins up to 5 mm. The left ovary has a pronounced expansion in the external parts.
- Second degree. This degree is characterized by the spread of pathology and damage to the left ovary. The veins of the uterus and right ovary can also be dilated. The expansion diameter reaches 10 mm.
- Third grade. The diameter of the veins increases up to 1 cm. The expansion of the veins is observed equally on the right and left ovaries. This phase is due to pathological phenomena of a gynecological nature.
It is also possible to classify the disease according to the primary cause of its development. There is a primary degree, in which the expansion is caused by a defective functioning of the venous valves, and a secondary degree, which is a consequence of chronic female diseases, inflammatory processes or complications of an oncological nature. The degree of the disease may differ according to the anatomical feature, which indicates the location of the vascular disorder:
- Intra-caste Plethora.
- Vulvar and perineal.
- Combined forms.
Symptoms and clinical manifestations
In women, pelvic varicose veins are accompanied by severe, but non-specific symptoms. Often, the manifestations of this disease are considered to be signs of gynecological disorders. The main clinical symptoms of varicose veins in the groin in women with pelvic vessel involvement are:

- Non-menstrual pain in the lower abdomen. Their intensity depends on the stage of venous damage and the extent of the process. For the 1st degree of varicose veins of the small pelvis, periodic and mild pain is characteristic, extending to the lower back. In the later stages, it is felt in the abdomen, perineum and lower back, and is long and intense.
- Abundant mucous discharge. The so-called leukorrhea does not have an unpleasant smell, does not change color, which would indicate an infection. The discharge volume increases in the second phase of the cycle.
- Increased symptoms of PMS and dysmenorrhea. Even before the onset of menstruation, the pain in women increases, leading to difficulties in walking. During menstrual bleeding, it can become unbearable, spreading to the entire pelvic region, perineum, lower back, and even the thighs.
- Another characteristic sign of varicose veins in the groin in women is discomfort during intercourse. It is felt in the vulva and vagina and is characterized as a dull pain. It can be observed at the end of the relationship. In addition, the disease is accompanied by increased anxiety, irritability and mood swings.
- As with varicose veins of the small pelvis in men, in the female part of patients with such a diagnosis, the interest in sex gradually disappears. The cause of the dysfunction is both constant discomfort and a decrease in the production of sex hormones. In some cases, infertility can occur.
Instrumental diagnostics
Diagnosis and treatment of varicose veins is performed by a phlebologist, a vascular surgeon. Currently, the number of cases of VVP detection has increased due to new technologies. Patients with CPP are examined in stages.
- The first stage is a routine examination by a gynecologist: acquisition of anamnesis, manual examination, ultrasound examination of the pelvic organs (to exclude other pathologies). Based on the results, an examination by a proctologist, urologist, neurologist and other related specialists is additionally prescribed.
- If the diagnosis is unclear, but there is a suspicion of VVPT, ultrasound angioscanning (USAS) of the pelvic veins is performed in the second stage. This is a non-invasive and highly informative diagnostic screening method used in all women with suspected VVPT. If previously it was believed that it was sufficient to examine only the pelvic organs (venous examination was considered difficult to access and optional), at present, ultrasound of the pelvic veins is a mandatory examination procedure. With the help of this method, it is possible to establish the presence of varicose veins of the small pelvis by measuring the diameters, the speed of blood flow in the veins and preliminary to find out what is the main pathogenetic mechanism: the failure of the ovarian veins or the venous obstruction. In addition, this method is used for the dynamic assessment of conservative and surgical treatment of VVPT.
- Research is carried out transvaginally and transabdominally. The parametric veins, inguinal plexuses and uterine veins are visualized transvaginally. According to different authors, the diameter of the vessels of the named localizations varies from 2. 0 to 5. 0 mm (on average 3, 9 ± 0, 5 mm), i. e. no more than 5 mm, and the average diameter of the arcuate veins is 1, 1 ± 0, 4 mm. Veins larger than 5 mm in diameter are considered dilated. The inferior vena cava, iliac veins, left renal vein and ovarian veins are examined transabdominally to exclude thrombotic masses and extravasal compressions. The length of the left renal vein is 6-10 mm, and its average width is 4-5 mm. Normally, the left renal vein at the point where it passes over the aorta is somewhat flattened, but a decrease in its transverse diameter by 2-2. 5 times occurs without a significant acceleration of blood flow, which ensures normal outflow without increasing the pressure in the pretenotic zone. In the case of stenosis of a vein against the background of pathological compression, there is a significant decrease in its diameter - by 3. 5-4 times, and an acceleration of blood flow - over 100 cm / s. The sensitivity and specificity of this method are 78 and 100%, respectively.
- Examination of the ovarian veins is included in the mandatory examination of the pelvic veins. They are located along the anterior abdominal wall, along the rectus abdominis muscle, slightly lateral to the iliac veins and arteries. A sign of ovarian venous insufficiency in USAS is considered to be more than 5mm in diameter with the presence of retrograde blood flow. For a comprehensive examination, prevention of recurrence and correct treatment tactics, ultrasound scans of the veins of the lower extremities, perineum, vulva, inner thigh and gluteal region should be performed.
- The development of medical technology has led to the use of new diagnostic methods. In the third stage, after ultrasound verification of the diagnosis, radiation diagnostic methods are used to confirm it.
- Pelvic phlebography with selective bilateral radiopaque ovarian imaging is one of the radio-invasive diagnostic methods that is performed only in a hospital setting. This method has long been considered the diagnostic "gold standard" for assessing dilatation and detecting valvular insufficiency in the pelvic veins. The essence of the method is the introduction of a contrast agent under the control of an X-ray installation through a catheter installed in one of the main veins (jugular, brachial or femoral) in the iliac, renal and ovarian veins. Thus, it is possible to identify anatomical variants of the structure of the ovarian veins, determine the diameters of the gonadal and pelvic veins.
- The retrograde contrast of the gonadal veins at the peak of the Valsalva test serves as a pathognomonic angiographic sign of their valvular insufficiency with visualization of strong expansion and tortuosity, respectively. This is the most accurate method for detecting May-Turner syndrome, post-thrombophlebitic changes in the iliac and inferior vena cava.
- When the left renal vein is compressed, perirenal venous collaterals are determined with retrograde blood flow in the gonadal veins, contrast stagnation in the renal vein. The method measures the pressure gradient between the left kidney and the inferior vena cava. Normally, it is 1 mm Hg. Art. ; gradient equal to 2 mm Hg. Art. , May suggest a slight compression; with a gradient >3 mm Hg. Art. aorto-mesenteric compression syndrome with hypertension in the left renal vein and > gradient can be diagnosed5 mm Hg. Art. is considered a hemodynamically significant stenosis of the left renal vein. The determination of the pressure gradient is an important element of the diagnosis, since, depending on its values, essentially different surgical interventions are planned on the veins of the small pelvis, which is very important in modern conditions. Currently, this study (with a normal pressure gradient) can be used for therapeutic purposes - for embolization of the ovarian vein.
- The next method of radiation is emission computed tomography of pelvic veins with erythrocytes labeled in vitro. It is characterized by the deposition of marked erythrocytes in the veins of the pelvis and the visualization of the gonadal veins, allows to identify the varicose plexuses of the small pelvis and dilated ovarian veins in various positions, the degree of pelvic venous congestion, the reflux of blood from the veins pelvic veins in the saphenous veins of the legs and perineum. Normally the ovarian veins are not contrasted, no accumulation of the radiopharmaceutical is observed in the venous plexuses. For an objective assessment of the degree of venous congestion of the small pelvis, the pelvic venous congestion coefficient is calculated. But this method also has disadvantages: invasiveness, relatively low spatial resolution, the impossibility of accurately determining the diameter of the veins, so at the moment it is not so often used in clinics.
- The videolaparoscopic examination is a valuable tool in the evaluation of the undiagnosed. In combination with other methods, it can help determine the causes of pain and prescribe the correct treatment. With varicose veins of the small pelvis in the ovarian region, along the round and wide ligaments of the uterus, the veins can be visualized in the form of cyanotic and dilated vessels with a thinned and tense wall. The use of this method is significantly limited by the following factors: the presence of retroperitoneal adipose tissue, the possibility of evaluating varicose veins only in a limited area, and the inability to determine reflux through the veins. Currently, the use of this method is justified from a diagnostic point of view in cases of suspected multifocal pain. Laparoscopy allows you to visualize the causes of CPP, such as outbreaks of endometriosis or adhesions, in 66% of cases.
Features of therapy
For the complete treatment of varicose veins of the small pelvis, a woman must follow all the recommendations of the doctor, and also change her lifestyle. First of all, attention must be paid to the loads, if they are excessively high they must be reduced, if the patient leads an excessively sedentary lifestyle, it is necessary to practice sports, take more frequent walks, etc.
Patients with varicose veins are strongly advised to adjust their diet, consume as little junk food as possible (fried, smoked, sweet in large quantities, salty, etc. ), alcohol, caffeine. It is better to give preference to fruits and vegetables, dairy products, cereals.
Also, as a prophylaxis for the progression of the disease and for medicinal purposes, doctors prescribe the use of compression underwear for patients with varicose veins.
Medicines
ERCT therapy involves several important points:
- get rid of the reverse flow of venous blood;
- relief of the symptoms of the disease;
- stabilization of vascular tone;
- improvement of blood circulation in the tissues.
Preparations for varicose veins should be taken in courses. The rest of the drugs, which play the role of painkillers, can be drunk exclusively during a painful attack. For effective therapy, the doctor often prescribes the following drugs:
- phleboprotectors;
- enzymatic preparations;
- drugs that relieve inflammatory processes with varicose veins;
- pills to improve blood circulation.
Operative treatment
It is worth recognizing that conservative methods of treatment give truly visible results mainly in the initial stages of varicose veins. At the same time, the problem can be fundamentally solved, and the disease can be completely eliminated only with surgery. In modern medicine, there are many variants of surgical treatment of varicose veins, consider the most common and effective types of operations:
- embolization of the veins in the ovaries;
- sclerotherapy;
- uterine ligament plastics;
- removal of enlarged veins by laparoscopy;
- locking of the veins in the small pelvis with special medical clips (clipping);
- crossectomy - ligation of the veins (prescribed if, in addition to the pelvic organs, the vessels of the lower limbs are affected).
During pregnancy, only symptomatic therapy of varicose veins of the small pelvis is possible. It is recommended to wear compression tights, taking phlebotonics on the advice of a vascular surgeon. In the II-III trimester, phlebosclerosis of the varicose veins of the perineum can be performed. If, due to varicose veins, there is a high risk of bleeding during spontaneous childbirth, the choice is made in favor of operative delivery.
Physiotherapy
The physical activity system for the treatment of varicose veins in a woman consists of exercises:
- "Bicycle". We lie on our back, throw our hands behind the head or place them along the body. Raising our legs, we perform circular movements with them, as if we were pedaling on a bicycle.
- "Birch". We sit face up on any hard and comfortable surface. Raise your legs and gently start them behind your head. Supporting the lumbar region with your hands and resting your elbows on the ground, slowly straighten your legs, lifting your body.
- "Scissors". The starting position is on the back. Raise your closed legs slightly above floor level. We spread the lower limbs to the sides, bring them back and repeat.
Possible complications
Why are varicose veins of the small pelvis dangerous? The following consequences of the disease are often recorded:
- inflammation of the uterus, its appendages;
- uterine bleeding;
- abnormalities in the work of the bladder;
- the formation of venous thrombosis (a small percentage).
Prophylaxis
In order for the varicose veins in the small pelvis to disappear as soon as possible and in the future the pathology of the pelvic organs does not recur, it is worth adhering to simple preventive rules:
- perform gymnastic exercises every day;
- prevent constipation;
- observe a diet in which vegetable fiber must be present;
- do not stay in one position for a long time;
- take a contrast shower of the perineum;
- so that varicose veins do not appear, it is better to wear exceptionally comfortable shoes and clothes.
Preventive measures aimed at reducing the risk of the occurrence and progression of varicose veins in the small pelvis boil down mainly to the normalization of lifestyle.




































